Reclaiming Mental Health: Moving Away From The Medical Mental Health Model

Agne Moses
Founder of Radical Thought | Published on July 06, 2025
Developed by George Engel in 1977, the Biopsychosocial Model is a holistic framework for understanding health and illness. It integrates biological, psychological, and social factors, arguing that no single factor (e.g., biology alone) can fully explain human health or disease.
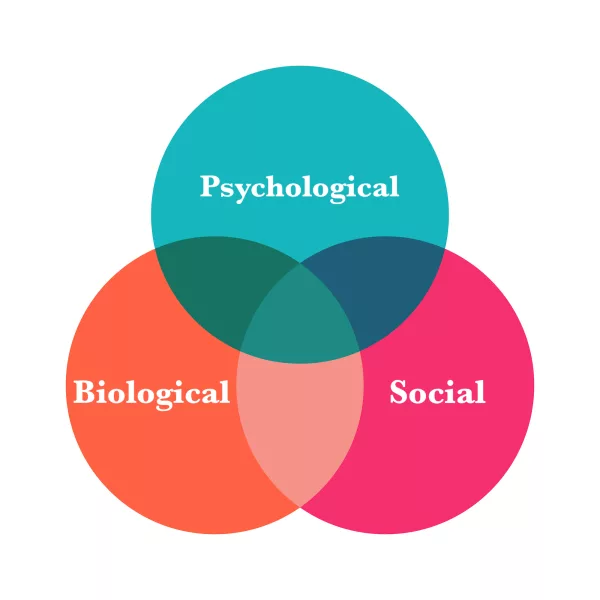
Biopsychosocial Model
Mental health has long been absorbed into the medical system- reduced to diagnoses, medications, and hospitalisations that often focus more on control than on true healing. But mental wellbeing is so much more. It’s a complex tapestry woven from our biology, psychology, and, most importantly, our social environments and lived experiences. In this blog, I explore how historical and modern mental health models have shaped what we believe about suffering and recovery- and why it's time to reclaim a more human, holistic, and empowering perspective.
"Through Radical Thought, I aim to challenge outdated mental health paradigms and advocate for systemic change rooted in lived experience, intersectional research, and community-driven solutions."
We start by asking a deceptively simple question:
Where does our mental health reside?
Many would instinctively point to the brain- understandable, given how often mental distress is framed as a “disease of the mind” or “disorder of the brain.” But that narrative doesn’t hold up when we look closely at the evidence, or listen deeply to real people's experiences. Science increasingly tells us what many of us know intuitively: mental health lives in the whole body, and is shaped by our relationships, environments, and lived realities. Behind every person in distress, there’s usually a web of context- chronic stress, poor physical health, broken relationships, trauma, or the daily struggle to meet basic needs like food and housing. Yet conventional psychiatry often overlooks this complexity. Instead of asking what happened to you?, it frequently asks what’s wrong with you? offering a diagnosis that places the problem inside the individual, while disregarding the broader social or structural causes of their distress. In doing so, it risks turning suffering into pathology and silencing the real stories behind people’s pain. To reduce this rich complexity to a “brain disease” is not only reductive- it’s misleading.
A Look Back: From Story to Symptom
The evolution of mental health documentation by Handerer et al (2020) in England and Wales from the mid-1800s to the modern NHS tells a powerful story:
1845–1900
English Asylum records were rich in social context, acknowledging grief, poverty, and life circumstances.

Picture by Dominic Lange Unsplash
1906 onwards
Introduction of coded diagnoses began to erase social causes, replacing them with biological labels like "hereditary insanity." This was the beginning of the system bureaucratisation, which has directly impacted erasure of social causes of distress in the records.
Picture by Jesse Orrico Unsplash
1913 Mental Deficiency Act
In 1913, the UK passed the Mental Deficiency Act, a law shaped by the eugenics movement’s troubling belief that society could be “improved” by controlling who was allowed to reproduce. This wasn’t just about care, it was about control. The Act introduced now-shocking diagnostic labels like “idiot,” “imbecile,” and “feebleminded,” often implying that these traits were hereditary and permanent. Many individuals, often poor, disabled, or socially marginalised, were institutionalized, not for treatment, but for segregation from society.

Picture by Hoshino Ai Unsplash
Post-1948 NHS:The Disappearance of Context
With the creation of the NHS in 1948, mental health care became more standardised, but also more medicalised. Psychosocial explanations for mental distress, factors like trauma, poverty, or family dynamics vanished from mainstream discourse. Instead, psychiatric diagnoses became self-contained: the label was both the cause and the condition. Suffering was no longer something to be understood in context- was something to be named, categorised, and medicated.

Picture by Towfiqu Barbuiya Unsplash
This shift marks the medicalisation of distress and a loss of narrative around why people suffer.
The Social Model of Disability, and its parallels and intersectionality with race and gender justice, reminds us of a vital truth: Many of the challenges we pathologise as “illness” are not inherent flaws within individuals, but the result of social barriers, systemic inequality, and exclusion. Yet, conventional approaches still try to treat these deep social wounds with medical bandages.
The takeaway?
To truly support wellbeing, we need to shift from asking "what's wrong with you?" to "what happened to you- and what's wrong with the systems around you?"
The Biopsychosocial Model: A More Complete Picture of Mental Health
It integrates three essential dimensions:
Although widely cited in theory, this model remains underutilised in real-world mental health care, where the biomedical approach still dominates.
It's time we embraced the biopsychosocial model not just as a concept, but as a practice- fully, consistently, and with compassion.
Final Thoughts: Towards a Person Centred Approach
Our understanding of mental health has too long been shaped by narrow, medicalised frameworks that pathologise distress and isolate individuals from the very context that shapes their experiences. But distress is not a malfunction, it’s a signal. A response to life’s circumstances, unmet needs, and systemic pressures. When we reduce this complexity to a diagnostic label, we risk erasing people’s stories and silencing the root causes of their pain.

Picture by Priscilla Du Preez Unsplash
Models like the Biopsychosocial and Social Model of Disability offer us richer, more compassionate lenses. They remind us that healing isn’t just about fixing brains, it’s about supporting people. It’s about addressing trauma, poverty, isolation, and inequality. It’s about creating environments where people can feel safe, connected, and seen. Let’s stop treating social wounds with only medical bandages. Let’s build systems that honour lived experience, restore dignity, and make space for human complexity.

About Agnė Moses
Psychology & Wellbeing Specialist challenging medicalised models of mental health. Founder of Radical Thought, creating inclusive, human-centred approaches that honour lived experience and promote true resilience. Currently completing a Master's in Research in Psychology of Mental Health and Wellbeing.