Mental Health Is Human: De-Medicalising Distress Through the Biopsychosocial Lens
The biopsychosocial model considers biological, psychological, and social factors in understanding mental wellbeing.
Last month, I had the privilege of presenting at a Be Well Lunch & Learn session hosted by the Music Publishers Association. My talk explored the concept of de-medicalising mental health, offering a range of holistic frameworks as alternatives to the dominant medical model. Together, we traced the historical shift toward medicalisation- shaped not just by science, but by political and bureaucratic forces. A key reference point was Handerer et al. (2020), whose study of Rainhill Asylum records illustrated how, by the 1950s, psychosocial explanations, such as grief or relational problems, for mental distress were almost entirely erased from mainstream policy and practice and NHS.
But the most powerful moments came not from theory, they came from real stories. In that room, we shared lived experiences that challenged dominant narratives. We spoke about resilience, identity, and the simple but radical idea that mental health should not be reduced to a diagnosis, because it is a dynamic spectrum of human experience. When someone asked why I got into mental health, I shared a piece of my personal journey.

Image by Redd Francisco Unsplash
But the most powerful moments came not from theory, they came from real stories. In that room, we shared lived experiences that challenged dominant narratives. We spoke about resilience, identity, and the simple but radical idea that mental health should not be reduced to a diagnosis, because it is a dynamic spectrum of human experience. When someone asked why I got into mental health, I shared a piece of my personal journey.
"What we often label as 'illness' can be simply explained by suffering, shaped by trauma, relationships, systems, and environments and expressed through coping, whether adaptive or maladaptive."

Image by Vitaly Gariev Unsplash
I grew up in an environment shaped by cycles of distress and instability, domestic violence, the kind that leave lasting marks across generations. About ten years ago, I found myself in a position where I had to take action to protect loved ones from harm. In the years that followed, I witnessed something remarkable: a close family member went through therapy and experienced a profound mindset shift. Until then, I believed, like many people, that change was rare, that character traits were fixed, and that mental illness was something you simply had to endure. But seeing that transformation firsthand challenged everything I thought I knew. It showed me that what we often label as "mental illness" may in fact be misunderstood suffering, shaped by trauma, systems, relationships, and environments, and expressed through coping, whether adaptive or maladaptive.
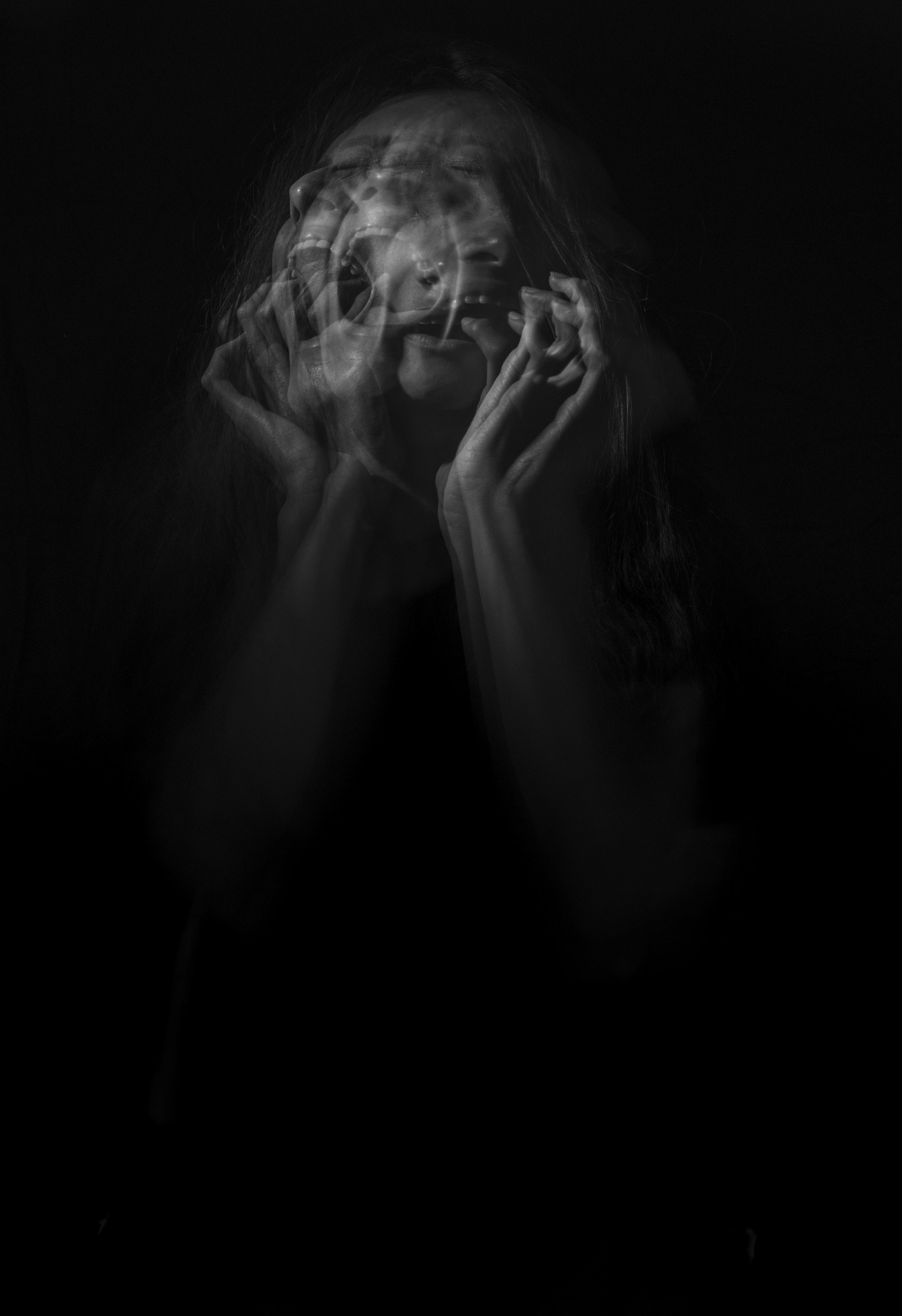
Image by Camila Quintero Franco Unsplash
The Power of Holistic Frameworks
One of the MPA attendees also shared their story. After receiving an MS diagnosis, they initially struggled with despair, until they began practicing elements of the biopsychosocial model without even knowing the name. Nourishing the body through food and exercise. Prioritising psychological care. Building social support. This model helped her reclaim agency, reminding us that health, mental or physical, is not just about biology. It's also about connection, movement, meaning, and community.

Image by Alexandra Tran Unsplash
Biological
Genetics, neurochemistry, physical health, medication effects, sleep, nutrition, exercise.
Psychological
Emotions, thoughts, coping skills, self-esteem, trauma history, personality traits.
Social
Relationships, culture, socioeconomic status, discrimination, life events, work environment.
That's what we explored together: How our systems have over-medicalised distress, and how holistic frameworks like the biopsychosocial and social constructionist models give us back a fuller, more human understanding of wellbeing.
We need models that honour lived experience, challenge rigid diagnostic labels, and hold space for both suffering and strength.
And we need to keep asking better questions. Let's keep challenging outdated narratives, and creating space for real, human transformation.
References:
Handerer, F., Kinderman, P., Timmermann, C., & Tai, S. J. (2020). How did mental health become so biomedical? The progressive erosion of social determinants in historical psychiatric admission registers. History of Psychiatry, 32(1), 0957154X2096852. https://doi.org/10.1177/0957154x20968522

About Agnė Moses
Psychology & Wellbeing Specialist challenging medicalised models of mental health. Founder of Radical Thought, creating inclusive, human-centred approaches that honour lived experience and promote true resilience. Currently completing a Master's in Research in Psychology of Mental Health and Wellbeing.